Glenoid Bone Loss in Degenerative Shoulder Conditions
What is Glenoid Bone Loss?
The shoulder joint has unique anatomic features because the socket portion of the joint is only a hollowed-out partial dish, with a depression similar to that of a golf tee. The shoulder socket (glenoid) has a surface anatomy that is less than an inch and a half wide(1), which means that because of its relatively small surface area, large forces are concentrated into it with shoulder activity. When we lift our arms to position the hand in space in front of us, the muscles work on the front of the arm to pull the humerus bone into position. This leads to a load on the shoulder joint that is directed posteriorly (backwards), which is why in individuals developing shoulder arthritis, the joint damage initially occurs at the back (posterior) part of the glenoid surface.
With shoulder osteoarthritis, the primary insult to the joint is the degeneration and wearing out of the cartilage lining. As that process progresses, the bones rub and the socket starts to undergo adaptive changes. These changes include hardening, cysts, and spurs, and are evident on radiographic imaging. As the arthritis becomes particularly severe, the joint shifts on itself and the ball begins to rub and grind on the back of the socket. Sometimes this will erode a second smaller socket in the back of the shoulder and the original bone becomes eroded and absent. This is called glenoid bone loss. When this occurs, the shoulder ball shifts posteriorly out the back of the socket (called subluxation), and is associated with substantial loss of function and range of motion. As this erosive process continues, the pain progresses and becomes associated with a profound loss of enjoyment of routine and sporting activities such as golf and tennis.
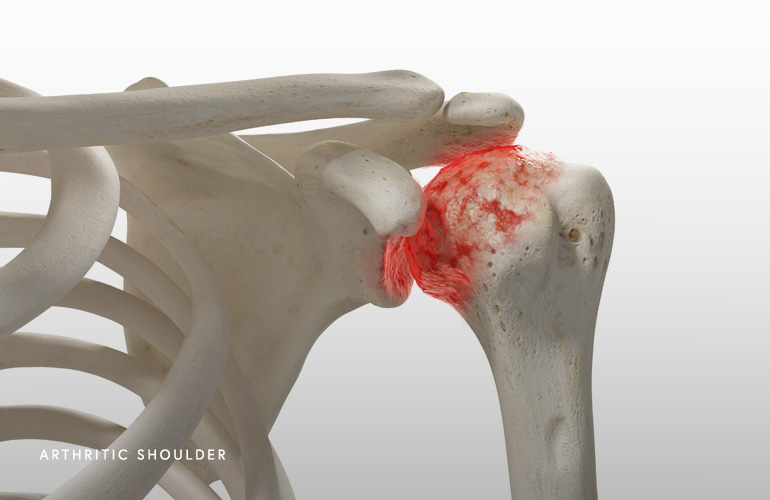
In 1999, Walch examined the CT scans of patients with shoulder osteoarthritis and classified arthritic and worn sockets into three categories: central wear, posterior wear, and dysplasia(2). Posterior wear, as above, is the most common. When posterior wear occurs, the shoulder can develop a second concavity or “new socket” because the shoulder shifts out the back first, then wears into a bone cavity. This wear and subluxation is important to evaluate by your doctor because it can affect treatment, and specifically needs to be address if you have surgery because it can affect the outcome of shoulder replacement.
The treatment of glenoid bone loss depends on several factors unique to the patient’s situation. First is the age and activity goals. Patients with primary osteoarthritis are typically candidates for total shoulder replacement, where strategies are used to either ream (correct) the version of the socket, to supplement the socket bone loss based on a sophisticated glenoid implant (“augment”) used at surgery, or based on the combination of the above. In patients that have very severe cases of glenoid bone loss, are older and may have limited activity demands, or have problems with the rotator cuff as diagnosed on imaging, reverse total shoulder replacement may be the best option. This is a discussion to have with shoulder surgeon Dr. Obermeyer if you have been deemed a candidate for shoulder replacement or have been struggling with pain and stiffness for some time.
If you have a tear in the rotator cuff or have a unique pattern of shoulder arthritis called cuff arthropathy, you may also have glenoid bone loss that requires indentification and proper treatment. In these conditions, reverse total shoulder replacement is typically appropriate which has better results than conventional replacement. In cuff tear arthropathy in particular, the shoulder undergoes characteristic patterns of wear(3), where the bone is eroded more superiorly (upper portion) in the socket. This typically requires correction with an augmented component or reshaping of the bone called reaming during replacement to ensure optimal long term results, pain relief, and recovery of function are achieved after surgery.
Shoulder surgeon Dr. Obermeyer uses advanced imaging with CT to generate a three-dimensional model of your shoulder blade and the architecture of the glenoid bone. Using CT scan not only allows the interpretation of the bone deep to the glenoid (the “vault”) but it permits evaluation of the position of the joint and humeral head in relation to the entire shoulder blade. This permits assessment of subluxation of the joint and a precise calculation of the position of the socket (called the “version”). These calculations and interpretation are important to complete preoperatively as it allows precise execution of the surgical plan to restore version and optimize soft tissue balance and component fixation at surgery. Using sophisticated software, Dr. Obermeyer is also able to select and plan components that are unique to your anatomy to optimize your outcome after shoulder replacement.
Schedule an orthopedic appointment
If you have symptoms consistent with Glenoid Bone Loss, call our office or book an appointment with shoulder surgeon Dr. Thomas Obermeyer. Dr. Obermeyer specializes in diagnosing and treating shoulder injuries. Dr. Obermeyer has orthopedic offices in Schaumburg, Bartlett, and Elk Grove Village, Illinois. Dr. Obermeyer regularly sees patients from throughout Illinois including Hoffman Estates, Palatine, Elgin, Streamwood, Arlington Heights, and Roselle communities.
- Mathews S, Burkhard M, Serrano N, Link K, Häusler M, Frater N, Franke I, Bischofberger H, Buck FM, Gascho D, Thali M, Serowy S, Müller-Gerbl M, Harper G, Qureshi F, Böni T, Bloch HR, Ullrich O, Rühli FJ, Eppler E. Glenoid morphology in light of anatomical and reverse total shoulder arthroplasty: a dissection- and 3D-CT-based study in male and female body donors. BMC Musculoskelet Disord. 2017 Jan 10;18(1):9. doi: 10.1186/s12891-016-1373-4. PMID: 28068966; PMCID: PMC5223371.
- Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999 Sep;14(6):756-60. doi: 10.1016/s0883-5403(99)90232-2. PMID: 10512449.
- Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004 Apr;86(3):388-95. doi: 10.1302/0301-620x.86b3.14024. PMID: 15125127.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

