Bankart and Hill Sachs Lesions
Traumatic shoulder instability is most commonly seen where the ball comes out the front of the socket, called anterior instability, and can cause injury to the shoulder joint on the humerus (ball) as well as on the glenoid (socket). Injuries such as a collision or a fall onto an outstretched arm are common mechanisms for traumatic instability. Anterior instability in the shoulder refers to a spectrum of abnormality, from subtle shifting motions called subluxations to more severe complete dislocations can tear tissues and ligaments and even cause fractures (breaks) to the bones. A detailed assessment of the bone and soft tissue anatomy is important if you have been diagnosed with anterior instability due to the potential for worsening damage to the shoulder joint and increasingly debilitating symptoms if left untreated.
Surgical treatment for anterior instability has evolved over the last few decades, from historically open and invasive surgery to most cases of anterior instability treated successful with more minimally invasive arthroscopy. Despite the overwhelming success and return to sport and activity with arthroscopic surgery, sometimes an open procedure is best, and it may be helpful to treat with a shoulder surgeon such as Dr. Obermeyer who is capable of offering all surgical options for anterior instability so he can guide you to the treatment that is best for your condition.
During an anterior shoulder dislocation, the front (anteroinferior) capsule and labrum is torn off from the front of the socket when the ball comes out. This injury is known as a Bankart lesion and is the most commonly observed soft tissue injury after subluxation or dislocation. The normal “bumper” effect of the labrum is gone with a Bankart lesion and the sealing effect of the labrum and ligaments are diminished when a Bankart lesion occurs. This lesion, when diagnosed, leaves the shoulder with a notable reduction in stability and leaves it prone to dislocating again.
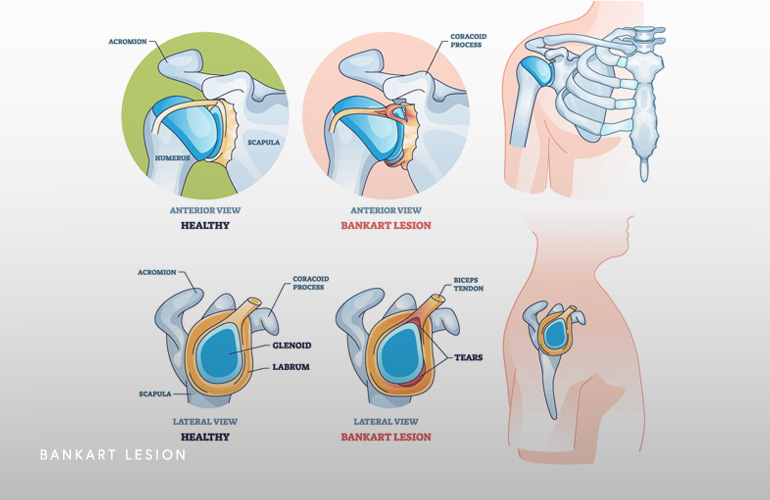
There is a variant of the Bankart lesion that occurs when a fracture occurs at the front of the socket (called a bony Bankart) that is an increasingly diagnosed condition in the setting of first time shoulder dislocation (as many as in one-third of cases in some studies[1]). When the bony Bankart fracture occurs, it is important to diagnose, as the bony piece can gradually erode, leaving a section of the front of the socket missing. This condition is called glenoid (socket) bone loss and leads to continued less of shoulder function and can require increasingly complex treatment when it occurs. Sometimes early arthroscopic surgery is recommended to repair the bony Bankart lesion when it occurs to prevent the development of glenoid bone loss.
The Hill-Sachs lesion is also considered a “compression” fracture, which is essentially a dent in the back of the ball as a result of it forcefully impacting the socket after it comes out. The Hill-Sachs lesion occurs in as many as 90% of patients after their first anterior shoulder dislocation. These lesions can involve just cartilage or both cartilage and bone, and when they occur, are important to understand because like glenoid bone loss, can greatly affect the risk of recurrence of a shoulder dislocation. The reason these lesions can contribute to instability is that they can often times “engage” or lock in the front of the socket when the arm is in an overhead position, increasing the risk of another dislocation.
The presence of a Bankart Lesion and a Hill-Sachs Lesion in the same shoulder has the potential for a “slippery slope” where both lesions contribute to susceptibility of the shoulder dislocating again. But it gets worse; each dislocation wears the bone out on the socket, worsening the glenoid bone loss, and increases the size of the Hill-Sachs Lesion. This process leads to worsening instability which can be very debilitating, affecting many activities. A common finding when this happens is the amount of force or injury that requires a dislocation to occur gets progressively minimal, and the shoulder can even start to dislocate in one’s sleep.
Treatment primary or recurrent instability with a Bankart lesion depends on risk of recurrence and activity expectations. Patients that are at risk of continued instability and are appropriate surgical candidates may be appropriate for repair of just the Bankart lesion itself and non-treatment of the Hill-Sachs Lesion. When the Hill-Sachs Lesion is small or the shoulder has only dislocated a few times, this arthroscopic Bankart repair procedure may be appropriate. This procedure has excellent clinical outcomes and is one of the most successful procedures in shoulder surgery.
When there is glenoid bone loss and a Hill-Sachs Lesion, the condition is called bipolar bone loss meaning there is a problem on both sides of the joint. In these cases there is more complex decision making to determine which treatment is appropriate. A new paradigm called the glenoid track is an imaging-based calculation of the contact area on the humeral head and the glenoid(2). The Hill-Sachs Lesion is considered to be off-track when it engages the front of the socket, otherwise it is considered on-track. When the Hill-Sachs Lesion is off-track, a procedure called a remplissage is typically added to the Bankart repair, which involves repairing part of the rotator cuff tendon into the Hill-Sachs Lesion so that it can no longer engage the glenoid. This procedure is also highly successful in appropriate patients.
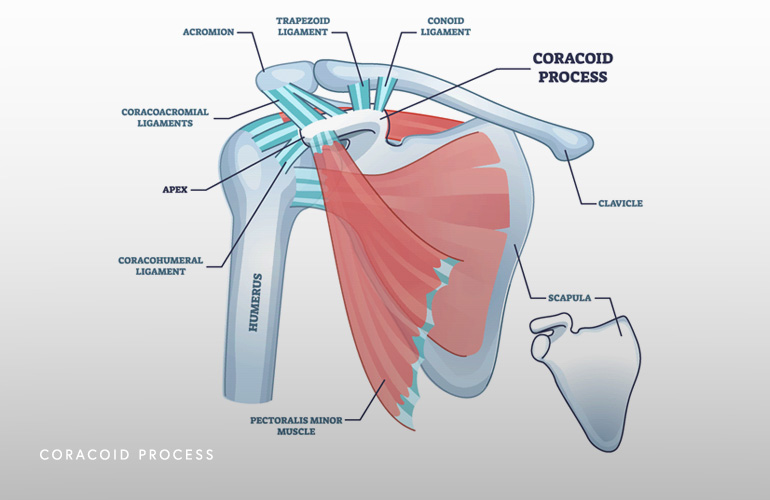
In more severe cases, when the glenoid bone loss is particularly severe, you had prior surgery that had failed, or if the Hill Sachs Lesion is large, you may be a candidate for an open procedure called the Latarjet. This procedure involves transferring bone from the shoulder blade (coracoid process) to the front of the socket to compensate for the bone loss and recruiting on of the rotator cuff tendons (subscapularis) to a sling to pull the head up into the socket. This procedure is more invasive and requires a detailed preoperative assessment to determine if it is right for you.
Historically, high level athletes or patients experiencing a first time dislocation were treated almost always nonsurgically, even in the presence of a Bankart lesion, because it was unclear about which patients would continue to struggle with function and the risks of surgery were higher at that time. As arthroscopic techniques evolved, the outcomes with arthroscopic primary repair are much better than before, and primary repair may prevent dislocation recurrence and the slippery slope of bone loss. For higher level contact athletes, primary repair of a Bankart lesion in the off season may result in higher levels of return to sport in the subsequent sporting season(3). This may be a difficult decision, and you can discuss your individual circumstances with Dr. Obermeyer to determine if arthroscopic surgery is right for you.
Schedule an orthopedic appointment
Are you or a loved one suffering from a Bankart and Hill Sachs Lesion? Call or make an appointment online with shoulder surgeon Dr. Thomas Obermeyer. Dr. Obermeyer is widely regarded as one of the best shoulder surgeons in Illinois. Dr. Obermeyer has orthopedic offices in Schaumburg, Bartlett, and Elk Grove Village, Illinois. Dr. Obermeyer regularly sees patients from throughout Illinois including Hoffman Estates, Palatine, Elgin, Streamwood, Arlington Heights, and Roselle communities.
- Nakagawa S, Iuchi R, Hanai H, Hirose T, Mae T. The Development Process of Bipolar Bone Defects From Primary to Recurrent Instability in Shoulders With Traumatic Anterior Instability. Am J Sports Med. 2019 Mar;47(3):695-703. doi: 10.1177/0363546518819471. Epub 2019 Jan 23. PMID: 30673556.
- Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, Okada K. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007 Sep-Oct;16(5):649-56. doi: 10.1016/j.jse.2006.12.012. Epub 2007 Jul 23. PMID: 17644006.
- Dickens JF, Rue JP, Cameron KL, Tokish JM, Peck KY, Allred CD, Svoboda SJ, Sullivan R, Kilcoyne KG, Owens BD. Successful Return to Sport After Arthroscopic Shoulder Stabilization Versus Nonoperative Management in Contact Athletes With Anterior Shoulder Instability: A Prospective Multicenter Study. Am J Sports Med. 2017 Sep;45(11):2540-2546. doi: 10.1177/0363546517712505. Epub 2017 Jun 28. PMID: 28657778.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

