Knee and Patellar Dislocation
A “dislocating knee” can be a descriptor placed on many forms of an unstable knee where the bones shift or move in relation to one another. Most common in this category is a patella (kneecap) dislocation where the kneecap pops out of position from the shallow (trochlea of the femur) groove at the front of the knee. Patellar dislocations can be predisposed by several anatomic factors and in some patients can cause recurrent episodes of shifting (subluxation) leading to discomfort, apprehension or fear of injury, and deterioration of athletic ability. Patellar dislocations and instability are common in younger and adolescent athletes. Quite rare is a true knee “dislocation” where the femur (thighbone) completely shifts in relation to the tibia (shinbone) which is only seen in severe accidents and is discussed elsewhere.
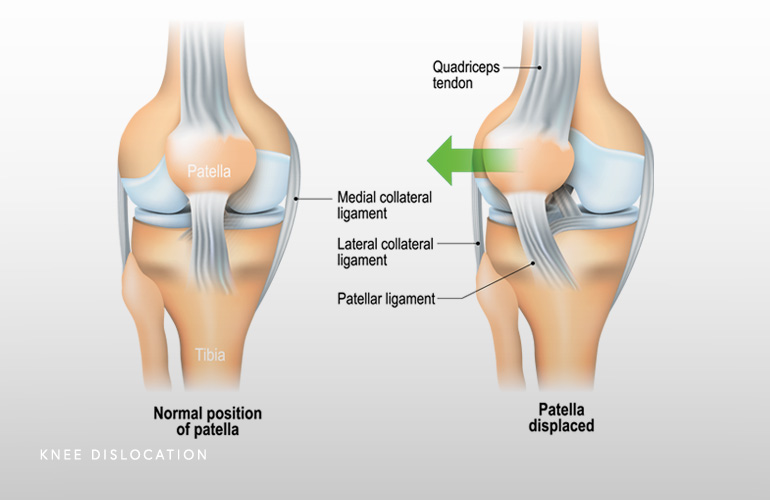
The patella is called a sesamoid bone because it is formed within the substance of the quadriceps tendon and functions to improve the mechanical advantage of the quadriceps muscle during knee extension (straightening). This mechanical feature allows us to generate tremendous loads across the knee and perform otherwise impossible feats like climbing stairs, running, and rising from a seated position. The quad tendon blends into the patella which then forms the patellar tendon, inserting onto the tibia.
The vector of pull of the quadriceps muscles naturally places a lateral (outside) force on the patella, which is increased in knee flexion, as when the foot is planted and the body shifts position forcefully, resulting in a lateral dislocation. When the patella laterally dislocates, the medial patellofemoral ligament (MPFL) and the medial retinaculum are necessarily injured.
When the kneecap dislocates laterally, there is typically a sensation of “giving way” or pop, followed by pain. Findings at the time of the dislocation can include swelling, tenderness around the kneecap area of the knee, and pain with attempted positioning of the leg. Radiographic evaluation is typically not needed and the kneecap sometimes spontaneously pops back into position or can be done so passively (from the patient’s point of view) by an onlooker.
The office evaluation of the recently dislocated patella is notable for swelling and pain, apprehension or guarding, and difficulty with weightbearing. X-rays should be performed to rule out a cartilage fracture (called an osteochondral lesion). Crutches and bracing are initially recommended but when the pain of the initial injury subsides, the shifting of the kneecap can be examined. Apprehension and popping or abnormal movement of the patella is evident (called the “J” sign). Often MRI is useful to check the extent of the soft tissue injury, to evaluate the bony anatomy (which can sometimes predispose to further dislocations), and to inspect the cartilage surfaces which can be injured during the dislocation or subluxation episode(s).
Once your anatomy is evaluated and the swelling and pain from a dislocation has subsided, you may be a candidate for a course of bracing and physical therapy/strengthening to improve the inner quadriceps muscle tone (called the vastus medialis obliquus) and improve the tracking of the kneecap so the injury does not happen again. Physical therapy is particularly helpful for the athlete with just a single dislocation. However, some patients may have repeated episodes of instability, particularly with lax or loose and injured medial soft tissue restraints (specifically the medial patellofemoral ligament and retinaculum), and these patients may be candidates for surgery to restore the injured and incompetent soft tissues. The increasingly utilized procedure for this condition is called medial patellofemoral ligament (MPFL) reconstruction.
Young age is one of the greatest risk factors for a recurrent dislocation, which is as high as 70 percent in some studies(1). Other factors such as general joint hypermobility, joint laxity, and certain bony (osseous) features (irregularity of the kneecap groove or trochlea, patella alta or high-sitting of the kneecap, among others) can also predispose to recurrent dislocations. If nonsurgical management fails, these patients may be candidates for soft tissue reconstruction called medial patellofemoral ligament (MPFL) reconstruction, which is a minimally invasive arthroscope-assisted procedure that restores the medial soft tissues around the knee. Medial patellofemoral ligament reconstruction performed by expert knee surgeon Dr. Thomas Obermeyer is a very successful procedure with recent improvements in the technology for graft anchoring and functional return(2). Uncommonly, patients with more substantial bony malalignment concerns (including an elevated distance between the trochlea or kneecap slot and the tibial tubercle where the patellar tendon inserts) require a realignment of the bones around the kneecap including a shifting of the kneecap tendon insertion point (called osteotomy).
Surgical treatment for soft tissue (medial patellofemoral ligament or MPFL) reconstruction is a minimally invasive same-day procedure which involves crutches and a brace, motion exercises, and muscle activation for about one month followed by return of normal walking and physical activity. Patients resume running by 3-4 months postoperatively and return to sports is complete by 4-6 months following surgery.
Schedule a knee consultation today.
A dislocating knee is a common condition affecting young athletes and in some can be a cause of athletic deterioration and pain. Expert knee surgeon Dr. Thomas Obermeyer treats these conditions routinely and will be able to provide guidance and sophisticated and modern surgical treatment only when necessary.
References:
- Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008 Mar;90(3):463-70. doi: 10.2106/JBJS.G.00072. PMID: 18310694.
- Smith BL, Bedi A, Hauck OL, Wijdicks CA, Riboh JC. All-Suture Anchor Onlay Fixation for Medial Patellofemoral Ligament Reconstruction: A Biomechanical Comparison of Fixation Constructs. Orthop J Sports Med. 2024 Nov 22;12(11):23259671241294011. doi: 10.1177/23259671241294011. PMID: 39583149; PMCID: PMC11585034.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

