Biceps Injuries at the Elbow
Injuries to the end (distal part) of the biceps tendon represent a detachment of the tendon insertion into the elbow at the radius. These injuries commonly affect men between the ages of 40 and 50 in the dominant elbow(1). Injuries to the tendon is frequently seen in active patients, with high athletic or occupational demands but not always. The tendon typically tears as a result of a forceful eccentric biceps contraction, where the muscle contracts while it lengthens. There is a correspondingly high load transmitted through the tendon at the attachment site, causing a tear.
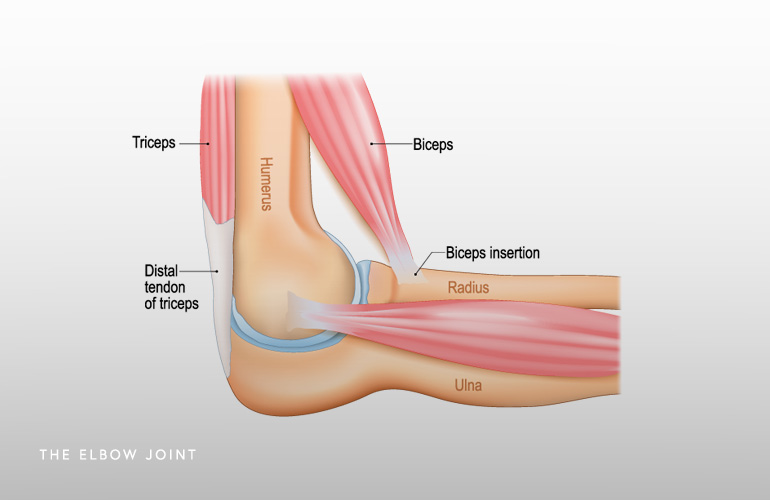
The anatomy of the biceps insertion at the elbow becomes important to understand as it relates to the restoration of the biceps attachment site when surgery is performed. The biceps tendon can be differentiated into two “heads” at the insertion site, with the more distal one performing more of an elbow flexion role and the deeper/ulnar one performing more of a pulling role on the radius bone, where it rotates the palm up (called supination). Restoring both heads is performed at the time of surgery, if elected, with the deeper/ulnar head being particularly important, as clinical deficits are likely to persist if the supination function of the biceps is not restored.
Patients experiencing a rupture of the distal biceps will frequently experience a “pop” at the elbow during a forceful lifting or pulling activity. There is typically pain and weakness experienced thereafter, particularly in supination, as well as deformity of the muscle belly of the biceps at the front of the arm. Bruising (called ecchymosis) is noted on the front and inner (medial) parts of the elbow. The diagnosis of a biceps rupture is a clinical one, and an experienced examiner will know if the tendon is torn.
Radiographs taken after a biceps injury are typically normal, and while not necessary to make the diagnosis, are often performed to rule out associated injuries to the bone or ligaments of the elbow. MRI is recommended in most cases. MRI will confirm the diagnosis in unclear cases, help to identify the extent of the tendon injury in the setting of partial ruptures, and help to identify the location of the tendon (how far it has pulled off/retracted) for surgical planning.
The preferred treatment recommendation for active patients who wish to preserve full function and restore full strength of the arm is surgical repair. While some patients who are less active and possibly older will tolerate nonsurgical treatment well, there will be permanent deficits in elbow flexion and forearm supination strength. Repairing the tendon surgically will improve flexion strength approximately 30% and supination strength approximately 40%(2). It is the supination strength deficit with nonsurgical management (noticed with pulling or twisting activities such as using a screwdriver) that is most noticeable. Elbow flexion strength is counterintuitively not as affected, in large part because there are other synergistic muscles that perform that flexion function (including the brachialis and brachioradialis).
Timing of surgery to reattach the biceps tendon is also an important consideration. If the decision for surgery is made, acute repair in the weeks following the injury is optimal. In these cases, the tendon is not scarred, has optimal mobility, and has a fresh track of retraction that can be followed surgically to place it back in the original anatomic position. In the setting of chronic ruptures or in cases when surgery is delayed, sometimes a more extensile incision or a second incision is required to retrieve and mobilize the tendon. In chronic cases with impaired tendon mobility, the tendon may have to be attached in a somewhat shortened position that requires a more delayed rehabilitative process to ensure the tendon can heal before being stretched with straightening (extending) the elbow.
Surgical reattachment of the distal biceps involves an incision in the front of the elbow that is a couple to a few inches long and involves spreading the muscles apart to identify and retrieve the tendon, followed by fixing the tendon to the bone of the radius using a button and/or a screw called an interference screw, which provides secure and robust fixation. Typically protected motion in a brace under the direction of a therapist is initiated within one week of surgery. There is a low risk of injury to blood vessels or nerves during the surgery, although that risk may be higher in select cases, and will be discussed with you during your preoperative consultation.
Schedule an orthopedic appointment
Are you or a loved one suffering from a biceps injury? Call or make an appointment online with elbow surgeon Dr. Thomas Obermeyer. Dr. Obermeyer is widely regarded as one of the best elbow surgeons in Illinois. Dr. Obermeyer has orthopedic offices in Schaumburg, Bartlett, and Elk Grove Village, Illinois. Dr. Obermeyer regularly sees patients from throughout Illinois including Hoffman Estates, Palatine, Elgin, Streamwood, Arlington Heights, and Roselle communities.
- Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985 Mar;67(3):418-21. PMID: 3972866.
- Baker BE, Bierwagen D. Rupture of the distal tendon of the biceps brachii. Operative versus non-operative treatment. J Bone Joint Surg Am. 1985 Mar;67(3):414-7. PMID: 3972865.
At a Glance
Dr. Thomas Obermeyer
- 15+ years of training and experience treating complex shoulder and sports medicine conditions
- Expert subspecialized and board-certified orthopedic care
- Award-winning outstanding patient satisfaction scores
- Learn more

